- 30
- APR


HOW MANY FREE FLAPS OR MICROSURGICAL PROCEDURES ARE SAFE IN ONE PERSON?
LIFE THROUGH PLASTIC SURGERY IN PURSUIT OF EXCELLENCE
SUCCESSFUL REHABILITATION FOLLOWING EXTENSIVE POST- TRAUMATIC, LIFE THREATENING LOSS OF THE ANTERIOR ABDOMINAL WALL, ANTERIOR WALL OF THE URINARY BLADDER, PUBIC SYMPHYSIS AND PUBIC RAMUS, PHALLUS, SCROTUM, TESTES AND UPPER HALF OF THIGH SOFT TISSUE (RIGHT AND LEFT)..,
MR. NAVNEET SOLGAMA. 45 Yrs. Male
A young man aged about 40 years, sustained extensive degloving injury following a run over accident in October 1994. The patient was hit by a speeding truck and was dragged on the road for over 10 meters, with possibly the patient caught between the front wheel of the truck between his two legs and body by the bumper. Patient was initially treated at a Surgical Center in Gujarat, wherein early re-succitation, wound debridement and Urinary catheterization was undertaken, before shifting to the Bombay Hospital. On admission, the patient was toxic, running high grade fever due to septicaemia and was in a very poor general condition.
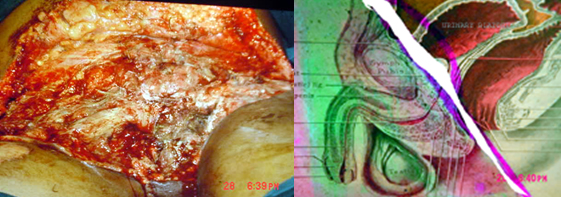
Contusion of the anterior abdominal wall, perineum and both thighs with an extensive laceration and loss of skin and subcutaneous tissue over thighs (anterio-medial aspect), perineal region with loss of penis & scrotum (including both testes) and lower half of the abdominal wall.
He was apparently hit and dragged on the road by a speeding truck, with the front wheel over his genitalia and the lower abdomen. Due to impact of the speed and the weight of the vehicle, the skin and the soft tissue over the medial, anterior and lateral aspects of both thighs, the perineum, groin and lower abdomen was badly crushed and avulsed.
The pubic symphysis and the 2/3 of the pubic rami with the phallus, scrotum, testis, bladder neck and the anterior part of the urinary bladder were missing. The patient was in a critical and morbid state and had lost all hopes for survival.
There were supra-pubic catheter and an indwelling urethral catheter, inserted earlier, however none of these catheters were draining. Two corrugated rubber drains were present on each side of thigh, but were not draining.
• There were # of both pubic rami with loss of pubic symphysis and pubic rami with # of ACETABULUM (R) with # of multiple ribs (L).
• Perineal indwelling catheter and supra-pubic catheter were not in the urinary bladder.
• Perineal indwelling catheter and supra-pubic catheter were not in the urinary bladder.
The Final Assessment of the tissue defect revealed:
• Extensive loss of skin, soft tissue and muscles of the anterior abdominal wall.
• Loss of the anterior wall of the urinary bladder.
• The urinary bladder lying open with edematous bladder mucosa and visible trigone.
• Extensive loss of skin and subcutaneous tissue over perineum and both thighs.
• Loss of penis and scrotum with both testes.
• Extensive loss of skin, soft tissue and muscles of the anterior abdominal wall.
• Loss of the anterior wall of the urinary bladder.
• The urinary bladder lying open with edematous bladder mucosa and visible trigone.
• Extensive loss of skin and subcutaneous tissue over perineum and both thighs.
• Loss of penis and scrotum with both testes.
It was not suitable to undertake ureteric catheterization to divert the urine due to fear of ascending urinary infection and damage to ureters. Nephrostomy was also not feasible as it would not have drained urine without distal obstruction.
The patient was continuously soaking his wound and dressings with urine. A low suction drainage was devised and kept in the perineum to suck out the urine from the trough.
The patient was continuously soaking his wound and dressings with urine. A low suction drainage was devised and kept in the perineum to suck out the urine from the trough.
Multiple major surgical reconstructions were carried out after reviving the patient. These are:-
A.
Repeated wound debridement and toileting
B. Thin Skin Grafts to the raw areas on abdomen and thigh (R+ L ).
C. EXTRA-CORPOREAL symbiotic radial artery forearm flap + vascularized osteotomised fibula graft for the perineal and pubic region to provide a stable and water resistant skin cover. Due to continuous dribbling of the urine, skin graft did float away.
The soft tissue defect in the perineum and the bony pubic defect were reconstituted with a symbiotic double flap transfer. An osteotomised vascularized fibula graft was used for the correction of pubic diastases and was fixed with mini-plates to part of the pubic rami on both sides . A distally based reversed radial artery forearm flap was designed and transferred as extracorporeal tissue transfer, to cover the vascularized bone graft and the perineal soft tissue defect. The vascular pedicle of the fibula graft was hooked on to the distal cut end of the Radial artery in the flap. Remaining raw areas over abdomen and both thighs were skin grafted.
The pedicle of the radial artery flap was divided after four weeks after confirming the vascularity of the flap by clamping the pedicle for six hours. Both flaps healed well and take of skin grafts over raw areas was good.
The use of a symbiotic flap allowed us to perform a complex reconstruction in an area, which was continuously being spilled by urine. Use of an extracorporeal tissue transfer technique, obviated the need to dissect femoral vessels in a badly crushed and infected tissue, as well permitted us to transfer two healthy and vascularized tissue flaps simultaneously.
After 4 months of the previous surgery, the general condition of the patient was much better. However, the patient still had the following problems:
The Urinary bladder was open difficult to locate the perineal urethra for diversion of urine.
Cystoscopy and urethroscopy performed through the opened urinary bladder revealed an intact trigone, neck and urethral sphincter. By a retrograde urethral catheterization, the distal perineal urethral passage was marked created and the meatus was opened by incising the transferred flap in the perineum. An indwelling urinary catheter was passed through perineal urethrostomy meatus thereafter. The catheter was allowed to remain in position for six weeks and moved up and down to facilitate creation of a good urethral passage.
After six weeks, bladder reconstruction was undertaken.
• The bladder wall from all sides was dissected and mobilized and closed in two layers with an indwelling urinary catheter.
• The bladder closure was reinforced with a gracillis muscle flap covered with skin graft.
D. Closure of the bladder and creation of the bladder neck and gracillis muscle flap for reinforcing the bladder closure.
E. Prefabricated phallus reconstruction, using extra-corporeal, symbiotic radial forearm flap and vascularized fibula graft.
F. Dynamic, innervated motor muscle transfer: Inferiorly based supercharged Lat. Dorsi muscle + island gracillis muscle flap for repair of lower abdominal wall and ventral hernia.
B. Thin Skin Grafts to the raw areas on abdomen and thigh (R+ L ).
C. EXTRA-CORPOREAL symbiotic radial artery forearm flap + vascularized osteotomised fibula graft for the perineal and pubic region to provide a stable and water resistant skin cover. Due to continuous dribbling of the urine, skin graft did float away.
The soft tissue defect in the perineum and the bony pubic defect were reconstituted with a symbiotic double flap transfer. An osteotomised vascularized fibula graft was used for the correction of pubic diastases and was fixed with mini-plates to part of the pubic rami on both sides . A distally based reversed radial artery forearm flap was designed and transferred as extracorporeal tissue transfer, to cover the vascularized bone graft and the perineal soft tissue defect. The vascular pedicle of the fibula graft was hooked on to the distal cut end of the Radial artery in the flap. Remaining raw areas over abdomen and both thighs were skin grafted.
The pedicle of the radial artery flap was divided after four weeks after confirming the vascularity of the flap by clamping the pedicle for six hours. Both flaps healed well and take of skin grafts over raw areas was good.
The use of a symbiotic flap allowed us to perform a complex reconstruction in an area, which was continuously being spilled by urine. Use of an extracorporeal tissue transfer technique, obviated the need to dissect femoral vessels in a badly crushed and infected tissue, as well permitted us to transfer two healthy and vascularized tissue flaps simultaneously.
After 4 months of the previous surgery, the general condition of the patient was much better. However, the patient still had the following problems:
The Urinary bladder was open difficult to locate the perineal urethra for diversion of urine.
Cystoscopy and urethroscopy performed through the opened urinary bladder revealed an intact trigone, neck and urethral sphincter. By a retrograde urethral catheterization, the distal perineal urethral passage was marked created and the meatus was opened by incising the transferred flap in the perineum. An indwelling urinary catheter was passed through perineal urethrostomy meatus thereafter. The catheter was allowed to remain in position for six weeks and moved up and down to facilitate creation of a good urethral passage.
After six weeks, bladder reconstruction was undertaken.
• The bladder wall from all sides was dissected and mobilized and closed in two layers with an indwelling urinary catheter.
• The bladder closure was reinforced with a gracillis muscle flap covered with skin graft.
D. Closure of the bladder and creation of the bladder neck and gracillis muscle flap for reinforcing the bladder closure.
E. Prefabricated phallus reconstruction, using extra-corporeal, symbiotic radial forearm flap and vascularized fibula graft.
F. Dynamic, innervated motor muscle transfer: Inferiorly based supercharged Lat. Dorsi muscle + island gracillis muscle flap for repair of lower abdominal wall and ventral hernia.
Total No. of Major Flaps used in one patient :
Seven
a. Radial Artery Forearm Flap : Extracorporeal : Two
b. Vascularized Fibula As Symbiotic flap : Two
a. Island Gracillis Muscle Flap : Two
b. Inferiorly based supercharged Latissimus Dorsi flap : One
a. Radial Artery Forearm Flap : Extracorporeal : Two
b. Vascularized Fibula As Symbiotic flap : Two
a. Island Gracillis Muscle Flap : Two
b. Inferiorly based supercharged Latissimus Dorsi flap : One
Due to regional advantage, these flaps either alone or in combination were carried out under regional anesthesia like Brachial block + Continuous Epidural block. The combinations allowed proper positioning of the patient while undertaking an extracorporeal tissue transfer. Lat. Dorsi muscle flap could also be dissected under thoracic epidural block along with infiltration in axilla for dissection of the pedicle.
Mr. Solgama has been finally discharged from the hospital after a total physical, functional and emotional rehabilitation and has gone back to the society full of self-confidence.
This patient is an example of perseverance and judicious use of surgical techniques and skills in a situation, which was definitely considered closer to death. Due Credit has been awarded to the Hospital set up and the Surgical team at the recently concluded International Conference of the Reconstructive Microsurgery, held at Singapore and Los Angeles, where in this patient was accepted and presented in the lecture " Limits in Microsurgery " as the maximum number of Microsurgical procedures being performed on an individual patient in the world literature, compiled by Dr. Baudet of France, the President of the International Society for Reconstructive Microsurgery.
This patient is an example of perseverance and judicious use of surgical techniques and skills in a situation, which was definitely considered closer to death. Due Credit has been awarded to the Hospital set up and the Surgical team at the recently concluded International Conference of the Reconstructive Microsurgery, held at Singapore and Los Angeles, where in this patient was accepted and presented in the lecture " Limits in Microsurgery " as the maximum number of Microsurgical procedures being performed on an individual patient in the world literature, compiled by Dr. Baudet of France, the President of the International Society for Reconstructive Microsurgery.